原文作者: Todd Hollingshead,
日期:2021年3月31日
翻译及注释:重返人生网
原标题:阿尔茨海默病的最新研究显示“一定程度上起源于生活习惯”
受阿尔兹海默症影响的大脑在使用葡萄糖的能力方面表现出遗传缺陷
多年来,确定阿尔茨海默症(AD)根本原因的研究一直集中在患者大脑中发现的斑块上。 但针对斑块聚集的治疗在恢复认知功能方面无效,这表明这种积聚可能是 AD 的副作用,而不是原因本身。(因果还是相关?)
美国杨百翰大学(BYU)研究人员团队的一项新研究发现了一种正在增强的替代理论在细胞水平上得到了新的支持:阿尔茨海默氏症实际上可能是大脑代谢功能障碍的结果。 换句话说,越来越多的证据表明饮食和生活方式是阿尔茨海默病的核心。
“阿尔茨海默症越来越多地被称为大脑的胰岛素抵抗或 3 型糖尿病,”高级研究作者、杨百翰大学生理学和发育生物学教授本杰明.比克曼博士说。 “我们的研究表明,至少在某种程度上,这种疾病可能与生活方式有关。”
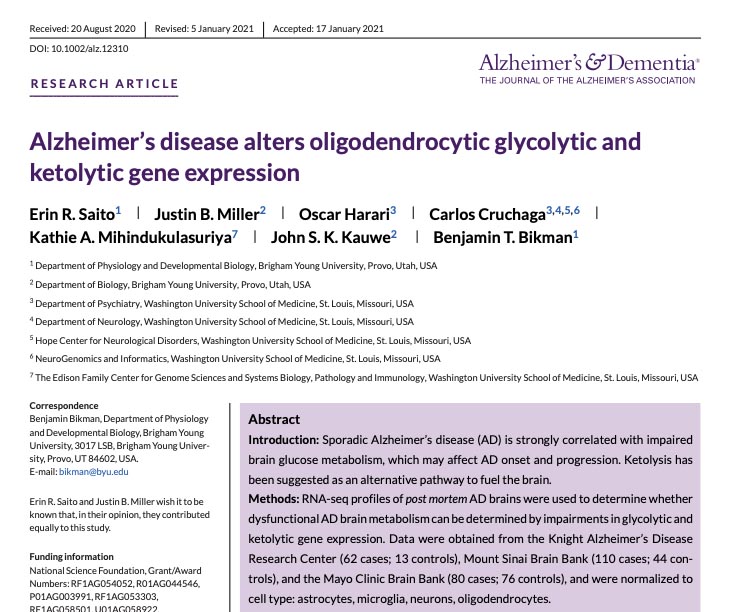
发表在学术期刊《阿尔茨海默症与痴呆症》(阅读论文,下载论文)上的这项新研究显示,BYU 研究小组检查了 240 个去世的阿尔茨海默症患者大脑中的 RNA 序列。 他们专门研究了两种代谢过程中神经系统支持细胞的基因表达:(1)葡萄糖代谢,碳水化合物被分解以提供能量的过程;(2)以及称为酮分解代谢的过程。
酮分解代谢中涉及到大脑从酮中获取能量,酮是胰岛素降低并且我们燃烧相对较多的脂肪时在我们体内产生的分子。 流行的“生酮饮食”以该过程命名,因为低碳水化合物、高蛋白饮食会降低胰岛素水平,并导致身体燃烧脂肪而不是碳水化合物,并且产生酮。
研究人员发现,前阿尔茨海默病患者大脑的那些神经系统支持细胞中存在广泛的葡萄糖代谢障碍,但酮分解代谢障碍有限。 这一发现意义重大,因为大脑就像一个混合引擎,能够从葡萄糖或酮中获取燃料,但在研究的阿尔茨海默氏症大脑中,大脑使用葡萄糖的能力似乎存在基本的遗传缺陷。
阿尔茨海默病潜伏发展的一个真正问题是,由于我们的饮食方式,绝大多数人从没有生过酮。 大多数人一直在吃含淀粉的食物,他们的胰岛素水平如此之高,以至于大脑在葡萄糖的海洋中挨饿
主要研究作者 ERIN Saito,三年级博士生,BYU
“我们已经将大脑的混合动力引擎变成了一个单一燃料系统,但它却无法正常运转,”比克曼博士说。 “因此,大脑在利用葡萄糖的能力方面逐渐变得不足,不断的在“求救”; 它在原本充足的养料中挨饿。 身体在葡萄糖的海洋中游泳,但大脑却无法使用它们。
“无法使用葡萄糖会增加酮的价值。 然而,由于普通人如此频繁地食用会刺激胰岛素的食物,因此大脑中从来没法利用任何酮,”Bikman 补充道。 “我将这一发现视为人为的问题,而且病症(的流行)正在变得更糟。”
先前的研究观察到,AD 患者的大脑吸收和使用葡萄糖的能力有可量化的降低,但本文首次证明它实际上发生在细胞层面。 对于阿尔茨海默病病因的研究而言,这是对治疗方式转变的重大贡献。
该论文得出结论:即使葡萄糖代谢失效,酮代谢似乎在 AD 患者中仍然保持正常,酮的治疗可能支持大脑代谢并减缓与疾病相关的认知衰退。
研究作者,包括首席研究员兼 BYU 教授 Justin Miller 和 BYU 教授 John Kauwe(现在也是 BYU夏威夷分校校长),建议未来研究阿尔茨海默病大脑代谢功能障碍的研究应该针对少突胶质细胞,因为在 AD 患者脑中的该细胞其基因在酮分解和糖酵分解中有差异表达。
这项研究是与圣路易斯华盛顿大学医学院的合作,后者为 BYU 研究团队提供了访问各种脑库的机会,包括梅奥诊所、西奈山和华盛顿大学的脑库。
生理学和发育生物学教授本·比克曼(BenBikman)和博士生艾琳·齐藤(Erin Saito)是一项研究代谢与阿尔茨海默病之间关系的资深和主要作者。
原文:
AD-stricken brains show a genetic deficit in ability to use glucose
For years, research to pin down the underlying cause of Alzheimer’s Disease has been focused on plaque found to be building up in the brain in AD patients. But treatments targeted at breaking down that buildup have been ineffective in restoring cognitive function, suggesting that the buildup may be a side effect of AD and not the cause itself.
A new study from a team of BYU researchers finds novel cellular-level support for an alternate theory that is growing in strength: Alzheimer’s could actually be a result of metabolic dysfunction in the brain. In other words, there is growing evidence that diet and lifestyle are at the heart of Alzheimer’s Disease.
“Alzheimer’s Disease is increasingly being referred to as insulin resistance of the brain or Type 3 Diabetes,” said senior study author Benjamin Bikman, a professor of physiology and developmental biology at BYU. “Our research shows there is likely a lifestyle origin to the disease, at least to some degree.”
For the new study, published in academic journal Alzheimer’s & Dementia, the BYU research team examined RNA sequences in 240 post-mortem Alzheimer’s Disease-impacted brains. They were looking specifically at the gene expression of nervous system support cells during two types of metabolism: glucose metabolism, where carbohydrates are broken down to provide energy, and something called ketolytic metabolism.
Ketolytic metabolism involves the brain creating energy from ketones, molecules made in our body when the hormone insulin is low and we are burning relatively higher amounts of fat. The popular “Keto Diet” is named after the process since that low-carb, high-protein diet lowers insulin levels and causes the body to burn fat instead of carbs and produce ketones.
The researchers found widespread glucose metabolism impairment in those nervous system support cells of the brains of former Alzheimer’s Disease patients, but limited ketolytic metabolism impairment. The finding is significant because the brain is like a hybrid engine, with the ability to get its fuel from glucose or ketones, but in the Alzheimer’s brains studied, there appears to be a fundamental genetic deficit in the brain’s ability to use glucose.
What we’re finding is that a real problem in the insidious development of Alzheimer’s Disease is that most people never have any ketones because of the way we eat. Most people are eating starchy meals all the time and their insulin is so elevated that the brain is starving in a sea of glucose.
LEAD STUDY AUTHOR ERIN SAITO, A THIRD-YEAR PH.D. STUDENT AT BYU
“We’ve turned the hybrid engine of our brains into a mono-fuel system that just fails to thrive,” Bikman said. “And so, the brain, which is progressively becoming deficient in its ability to use glucose, is now crying out for help; it’s starving in the midst of plenty. The body is swimming in a sea of glucose, but the brain just can’t use it.
“The inability to use glucose increases the value of ketones. However, because the average person is eating insulin-spiking foods so frequently, there’s never any ketones available to the brain,” Bikman added. “I look at these findings as a problem we’ve created and that we’re making worse.”
Previous research has observed that the brains of people with AD have a quantifiable reduction in the ability to take in and use glucose, but this paper is the first to show it actually happens at the cellular level. It’s a significant contribution to the growing paradigm shift in regards to the scientific view of the causes of Alzheimer’s.
And since ketolytic metabolism seems to keep working fine in people with AD, even when glucose metabolism gives out, the paper concludes that treatments involving ketones may be able to support brain metabolism and slow the cognitive decline associated with the disease.
Study authors, which include fellow principal investigator and BYU professor Justin Miller and BYU professor John Kauwe (also now president of BYU-Hawaii), suggest future research investigate metabolic dysfunction in Alzheimer’s Disease brains should target oligodendrocytes because genes involved in ketolysis and glycolysis are both differentially expressed in that cell type in AD brains.
This study was a collaboration with Washington University School of Medicine in St. Louis, who provided the BYU research team with access to various brain banks, including Mayo Clinic, Mount Sinai, and a brain bank at Washington University.
原文链接:https://news.byu.edu/new-research-on-alzheimers-disease-shows-lifestyle-origin-at-least-in-some-degree